
Economic Q&A replay: Light at the end of the Covid-19 tunnel
Following the announcement that the UK had approved a coronavirus vaccine for public use, we welcomed back Professor Michael Barrett of the Institute of Infection, Immunity and Inflammation at the University of Glasgow. He joined Investec's chief economist, Philip Shaw, in our latest webinar to give his insight as Britain begins to chart a path out of the pandemic.
Watch the full replay below, or click here to read the summary:
Q&A with the panel
- Professor Barrett answers questions on the effectiveness, rollout and safety of Covid-19 vaccines; the outlook for social restrictions; anti-vaccine sentiment; and tackling pandemics in the future. Philip Shaw also addresses questions on the UK economy, the inflation outlook and the prospects for US government stimulus.
If you don't receive invites already, please sign up here to receive invitations for upcoming webinars
Vaccine approval provides a route back to normality
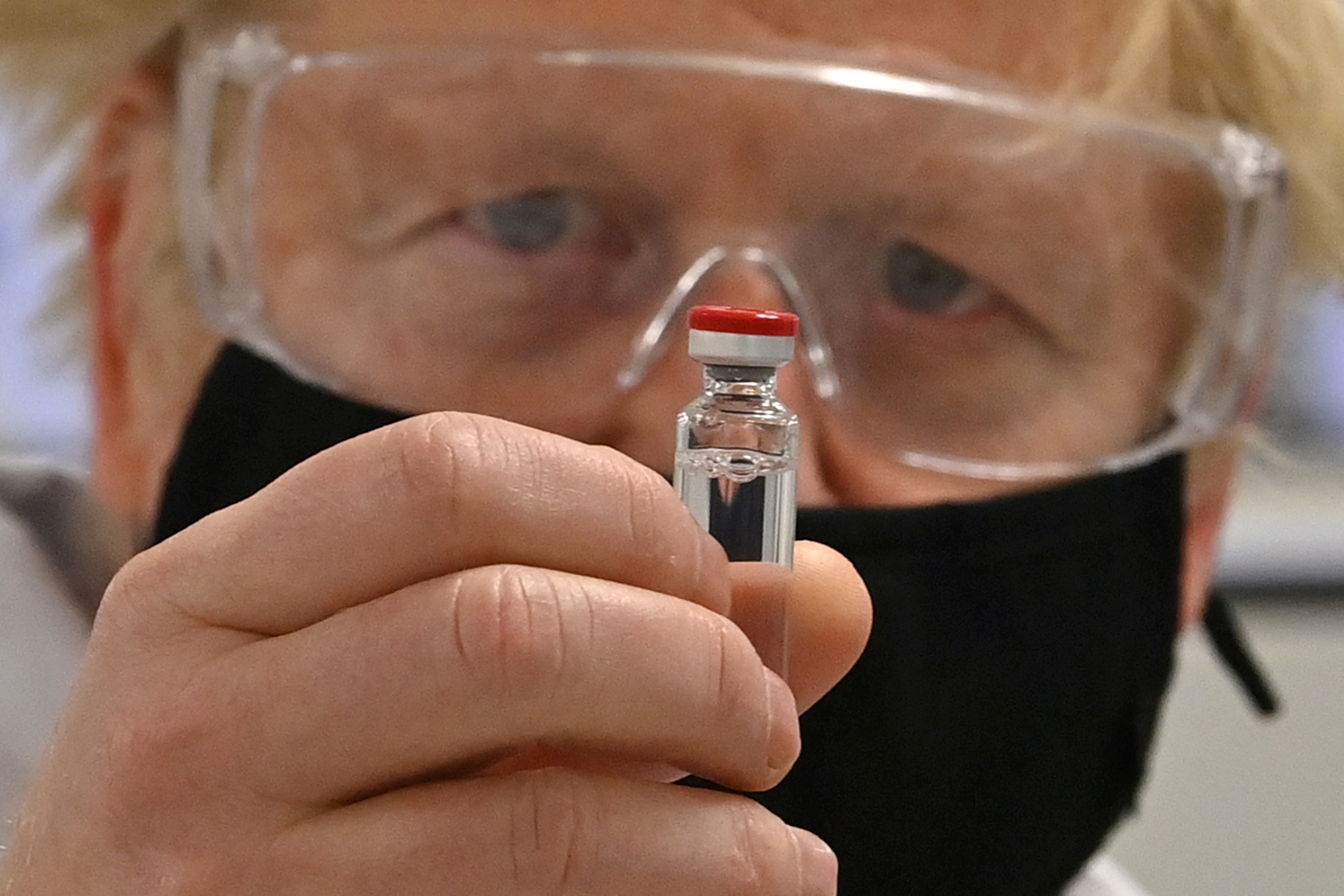
The announcement that the UK has become the world’s first country to approve the Pfizer/BioNTech coronavirus vaccine has finally given Britons some “light at the end of the tunnel”, said Professor Barrett.
“The announcement paves the way for a mass vaccination and means we now have a definitive and effective exit strategy. With a staged and successful rollout of the vaccine, we can return to normality in 2021. This is momentous news and testament to the unprecedented and collaborative response by the global scientific and medical community.
“This and other vaccines are likely to deliver many months of immunity and we can also look at providing boosters to ensure a longevity of response to the virus.”
Not out of the woods yet

While Professor Barrett was optimistic that progress on vaccines would finally provide a way out of the health crisis, he cautioned that “we are not out of the woods yet”.
“We still have some dark months ahead, and tragically, people will still get sick and die despite salvation being at hand. We must remain vigilant and continue to maintain high levels of restrictions and keep in place social distancing measures until the vaccine has shielded the vulnerable and we have sufficient numbers of people vaccinated.
“The reality is that we remain in the grip of a global calamity. Around 1.6 million people in the UK have been officially documented as infected (but true infections are thought to exceed 10 million) and 60,000 people have died. Despite the positive impact of the most recent lockdown, deaths have not come down as hoped.”
Given this challenging backdrop, Professor Barrett said it was his view and the consensus among public health officials that the tiered system must continue. “Until the vaccine rollout delivers a safe passage and herd immunity, many vulnerable people are still at risk.”
Also, there is a need for more data on whether the vaccines will stop people transmitting Covid-19, even if they remain uninfected or asymptomatic, and the vaccines can’t be used to treat people who already have the infection.
The logistical challenge
Rolling out such a mass scale vaccination requires a war-time collaborative effort. There will be challenges, both from a logistical and educational perspective, said Professor Barrett.
“There are many logistical variables, including manufacture and distribution. In the case of the Pfizer/BioNTech vaccine, it has to be moved up and down the country in a controlled way at minus 70 degrees Centigrade. We also need to roll it out while we keep restrictions in place.”
Still, the AstraZeneca/Oxford vaccine – which has yet to receive regulatory approval – is more robust and only needs to be kept at fridge temperature.
"We now have a definitive and effective exit strategy. With a staged and successful rollout of the vaccine, we can return to normality in 2021." -- Professor Michael Barrett
Tackling disinformation
“The reality is that vaccines are tested to be safe”, said Professor Barrett. But we still need to have “an unrelenting honest and clear programme of education around why vaccines work and what are the potential side effects to demonstrate that the positives vastly outweigh the negatives.
“There are real challenges around education. There is a vocal minority and they might impact an already difficult task of getting enough people inoculated to create herd immunity, which is estimated to happen once around 70% of the population have immunity, assuming all social distancing measures are removed.
“It is a battle of information and we may need to set in place legislation against the malicious spread of false or misleading information. Ultimately you are introducing an “S” or spike protein, which doesn’t do anything else to us other than prime an immune response to a coronavirus.”
Professor Barrett also said that for those with suppressed immune responses, the good news is these vaccines have removed the machinery for the viruses to replicate. If there are any adverse responses, they should be picked up in trials.
Improved testing success
Professor Barrett said testing had continued to improve. “We are now doing nearly half a million tests a day using the PCR (polymerase chain reaction) method. We have also seen the lateral flow community test in action. While this latter testing method is only 75% effective, it has a positive impact. When people are testing positive - even those who are asymptomatic - they now understand the problem of transmission and are self-isolating.”
Future-proofing against further pandemics
Professor Barrett said the UK has also begun setting up so-called megalabs, with one being created in England and another in Scotland. “While the impact of the Covid-19 pandemic has been grave, we must realise that we could have endured an even worse catastrophe. The megalabs may not have a huge impact on Covid-19 at this stage, but we need to have the capacity to look for further epidemics if they hit the UK.”
Limited success in drug therapy
The fight against Covid-19 in hospitals has also enjoyed some success. Professor Barrett said that while remdesivir has become well known following its use in treating US President Donald Trump, its efficacy seems limited to a relatively early stage of Covid-19 infection. Also, Regeneron’s antibody cocktail appears useful as they are similar to the antibodies individuals naturally produce against the virus.
Meanwhile, convalescent serum, where the antibodies of the infected can be purified and given to other people, isn’t working quite as well as hoped. However, the steroid dexamethasone remains the most effective treatment for those with serious late-stage conditions, which are due more to our response to the virus, rather than the virus itself. Overall, the picture hasn’t changed a great deal in recent months.
A quantum leap for vaccine development
Professor Barrett said it was clear early on that Covid-19 wasn’t changing in the same way that some other viruses evolve – something that makes producing a vaccine easier. It was also apparent within just a few months that these new, fast-tracked vaccines were inducing our immune systems to mount a sufficient response to the virus.
“Vaccines teach our immune systems to detect bugs that can avoid our immune systems. What we have done, traditionally, is take those bugs and weaken them so we can put them into a person so that the body will recognise the bug, but the weakened bug, will not cause the disease – or we kill the bug and put the dead pathogen into our body so it can recognise antigens, and this means we mount an immune response without risking infection with a live pathogen.”
However, Professor Barrett said these approaches are very time consuming and need dangerous pathogens for cultivation. “For decades we have been getting an influx of emerging infectious diseases, including the SARS outbreak in 2003, swine flu in 2009, Zika and Ebola. A number of influential people were of the opinion we need to do something different in developing vaccines. We couldn’t afford to take ten years to develop an effective response and so began the vaccine race.”
Back in 2017, the World Economic Forum, and a group of people led by Bill Gates and various governmental officials, created the Coalition of Epidemic Preparedness Innovations to fund scientists and organisations in new ways to develop vaccines with new technologies that could bypass having to use pathogenic microorganisms themselves.
And they began funding firms like Moderna to make RNA vaccines, where instead of taking a virus, they made an RNA, which is able to create antigens or proteins from the pathogen, without having to expose us to the pathogen itself. They funded Innovia to make a DNA-based vaccine and Oxford’s early research. These novel innovations laid the groundwork for the incredible vaccine race that started more or less immediately following the publication of the SARS CoV-2 coronavirus sequence within just a couple of weeks of identifying this new disease. All new vaccines are focusing on the “S” spike protein of the virus that sits on its surface and is the ideal target against which to mount that crucial immune response.
Read more articles from Investec Focus
Browse articles in
Please note: the content on this page is provided for information purposes only and should not be construed as an offer, or a solicitation of an offer, to buy or sell financial instruments. This content does not constitute a personal recommendation and is not investment advice.
